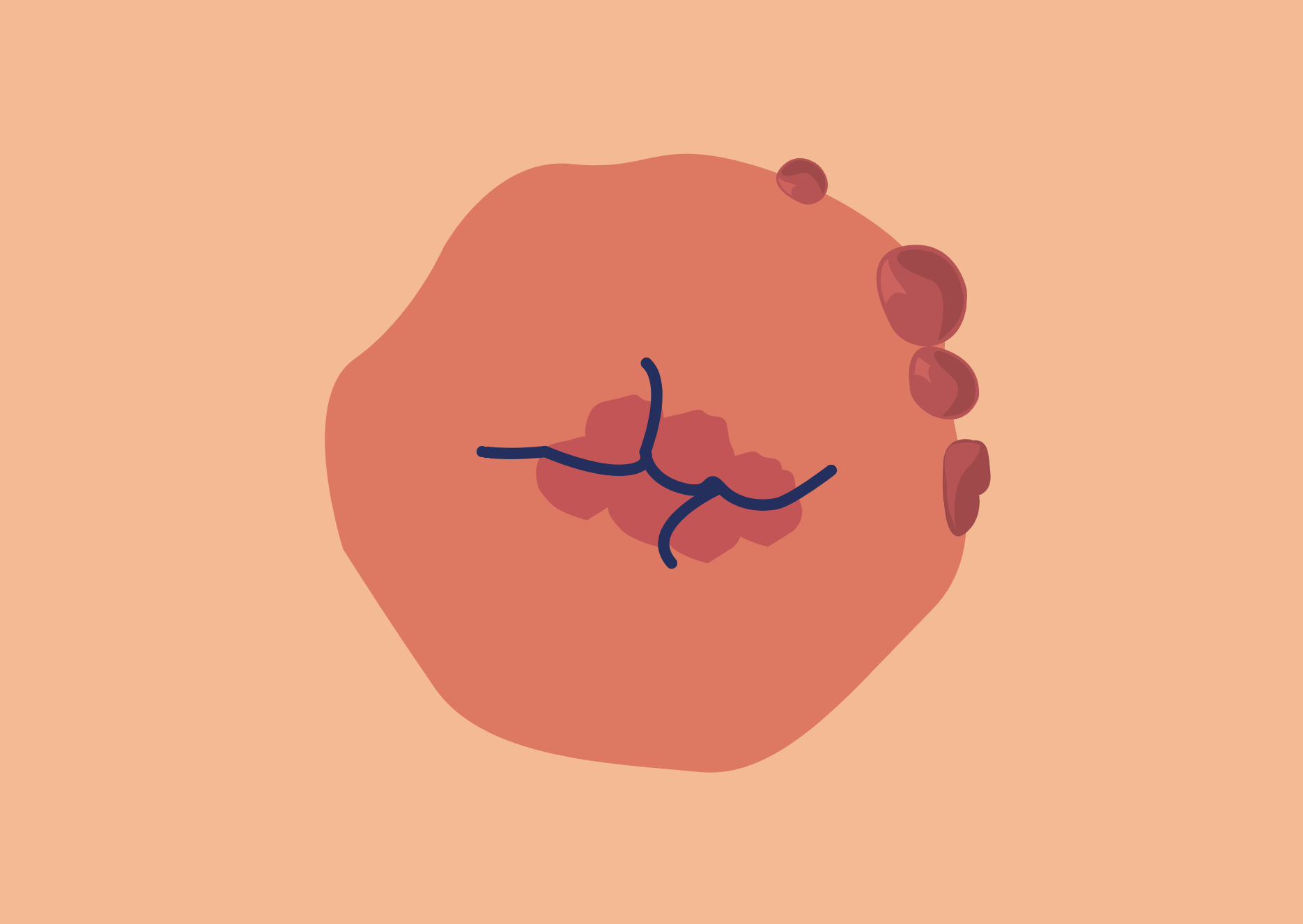
The exact cause is often unknown2, but infections, inflammation, irritants, and foreign objects are all common contributors for stoma granulomas. These can include:
- Sutures – from retained fragments, or a reaction to the suture material1,2,4
- Repeated trauma – from the opening of the ostomy appliance and/or the patient’s application or removal technique2,5
- Chronic irritation – from exposure to faecal output2,5,6,7
- Tight clothing or belts – which create friction in and around the mucocutaneous or stomal area.2
- An allergic reaction – to the stoma bag material5
Tips for preventing and managing granulomas
Although silver nitrate (which cauterises granulomas) is the most common treatment option for stoma granulomas, you can also help your patients make effective choices to minimise irritation and even prevent granulomas from occurring in the first place. These include:
- Decreasing friction and trauma (to prevent bleeding)2
- Making sure their ostomy appliance fits correctly – resizing the stomal opening if you need to, or adding an ostomy seal2,3,4
- Applying a barrier paste to the mucocutaneous junction2
- Avoiding tight fitting clothing and belts over the peristomal and stomal area2
Guidance and resources
We’ve gathered the latest data to help you, and your patients, manage stoma granulomas. You’ll also find tips for preventing them, and the innovative eakin® products that can help.
eakin® seals and granulomas booklet
Find out how eakin® seals have helped stoma care nurses to successfully manage previously problematic stoma granulomas.
eakin freeseal® for managing granulomas case study
See the data on how switching to an eakin freeseal® has impacted the quality of life for a patient experiencing peristomal skin complications and hypergranulation.
eakin Cohesive® stomawrap case study
Gain an insight into how our eakin Cohesive® stomawrap has prevented leaks and halved the number of changes for an active patient with a challenging stoma.
References
1. Beitz, J. M., & Colwell, J. C. (2014). Stomal and peristomal complications: Prioritizing management approaches in adults. Journal of Wound, Ostomy and Continence Nursing, 41(5), 445–454.
2. Johnson, T. (2010). Problematic stomas…Stoma granulomas. Colostomy Association Tidings Magazine.
3. Salvadalena, G. (2016). Peristomal skin conditions. In J. E. Carmel, J. C. Colwell, & M. T. Goldberg (Eds.) Wound, Ostomy and Continence Nurses Society core curriculum: Ostomy management (pp. 176–190). Philadelphia, PA: Wolters Kluwer.
4. Wound, Ostomy and Continence Nurses Society. (2010). Management of the patient with a fecal ostomy: Best practice guidelines for clinicians. Mt. Laurel, NJ: Author.
5. Dukes, S., Lowther, C., Martin, T., & Osborne, D. (2010). Guidelines for treating stoma granulomas at the mucocutaneous junction. Gastrointestinal Nursing, 8(1), 16–21.
6. Burch, J. (2014). Care of patients with peristomal skin complications. Nursing Standard, 28(37), 51–57. http://dx.doi.org/10.7748/ns.28.37.51.e8317
7. Lyon, C. C., & Beck, M. H. (2012). Chapter 97. Skin problems in ostomates. In L. A. Goldsmith, S. I. Katz, B. A. Gilchrest, A. S. Paller, D. J. Leffell, & K. Wolff (Eds.), Fitzpatrick’s Dermatology in General Medicine, 8e.
Ostomy products you can rely on

From pouches and seals to innovative accessories, our eakin® product range includes everything you need to support your patients after they’ve been discharged. You can order product samples directly from us or through your local rep to see the difference for yourself.